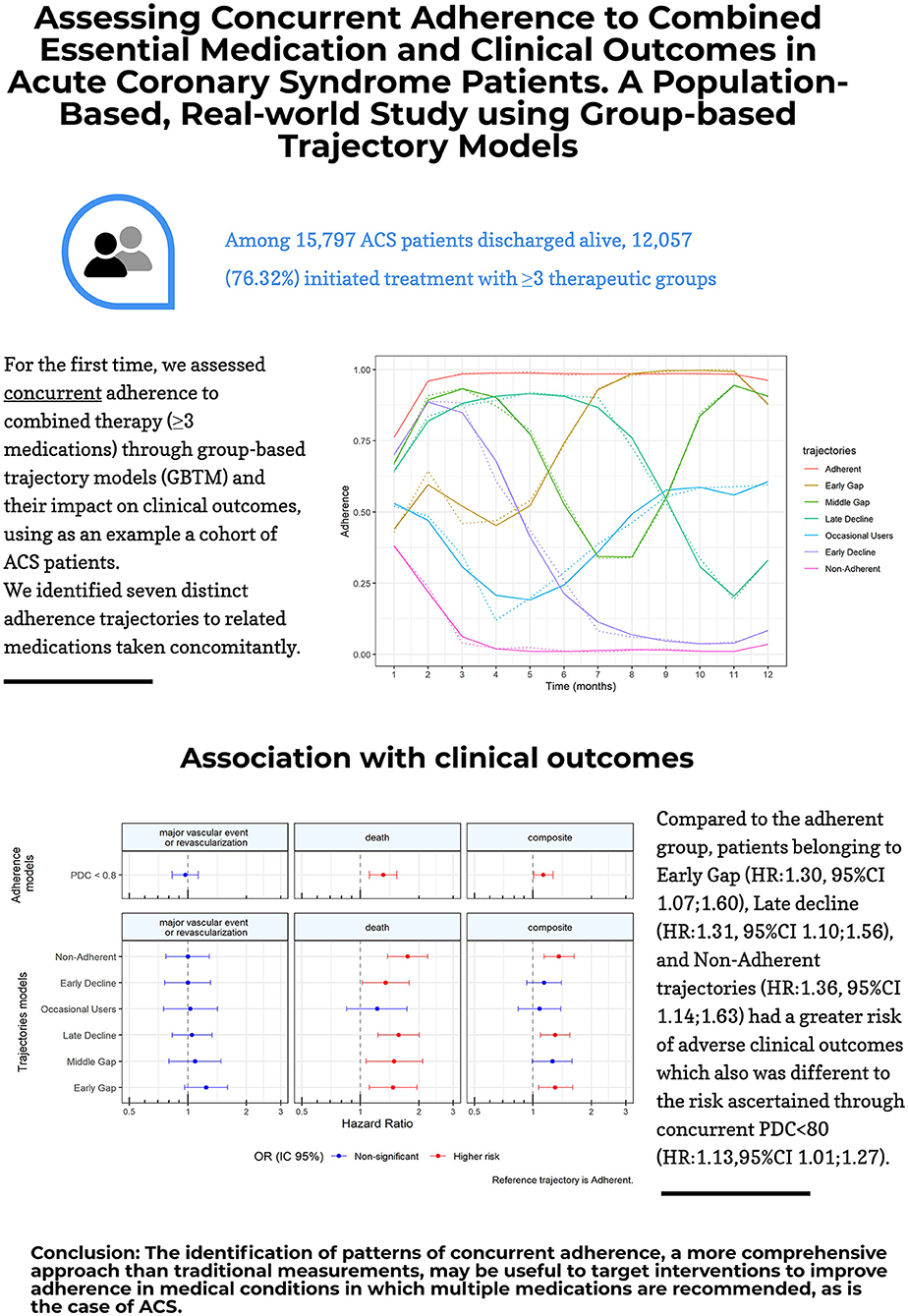
Therapeutic adherence to medication in patients with acute coronary syndrome (PREV2CI).
| | |
Objective | -
Assess therapeutic adherence with the classic measures of primary and secondary adherence (PDC and persistence) in a population environment of routine clinical practice of patients of both sexes aged 35 years and over discharged alive from any hospital of the Valencian Health Agency with a primary diagnosis of ACS. -
Assess the impact of non-adherence on the occurrence of clinical events. |
If you want to obtain more information about this project, collaboration possibilities and any other query related to this, you can contact us here.